Treatment of Eye Floaters
In the past, it was common practice for eye care professionals to advise patients to simply adapt to the presence of eye floaters and cope with the disturbance they create, and this approach remains prevalent today. This practice is justified by the fact that floaters are generally considered as harmless visual anomalies.
However, in recent years, there has been a notable shift in perspective, with a growing recognition of the impact of floaters on patients’ lives. The emphasis has expanded beyond the mere development of floaters to encompass a deeper understanding of their underlying causes. Furthermore, attention is now directed towards exploring options such as dietary and surgical interventions aimed at reducing the impact of floaters on patients’ quality of life. There is a growing recognition of the psychological and visual challenges faced by patients afflicted with floaters, who find it difficult to ignore or adapt to their presence, leading to a reevaluation of their significance.
On this page you will find four common treatment methods for eye floaters as well as their advantages and risks.
Taking No Action on Floaters
This approach is rooted in the medical consensus that floaters pose minimal risk, with eye care professionals primarily focused on monitoring symptoms that may indicate more serious conditions like retinal detachment.
Risks and Suitability of “Taking No Action on Floaters”
Choosing not to take action avoids the potential risks associated with surgical intervention. But Floaters are caused by degeneration of the vitreous. Ignoring them means not addressing or reversing the degenerative effect. With new lifestyle and nutrition-based non-inversive methods the “Take no Action” approach might be considered outdated.
Proactive Diet and Supplementation
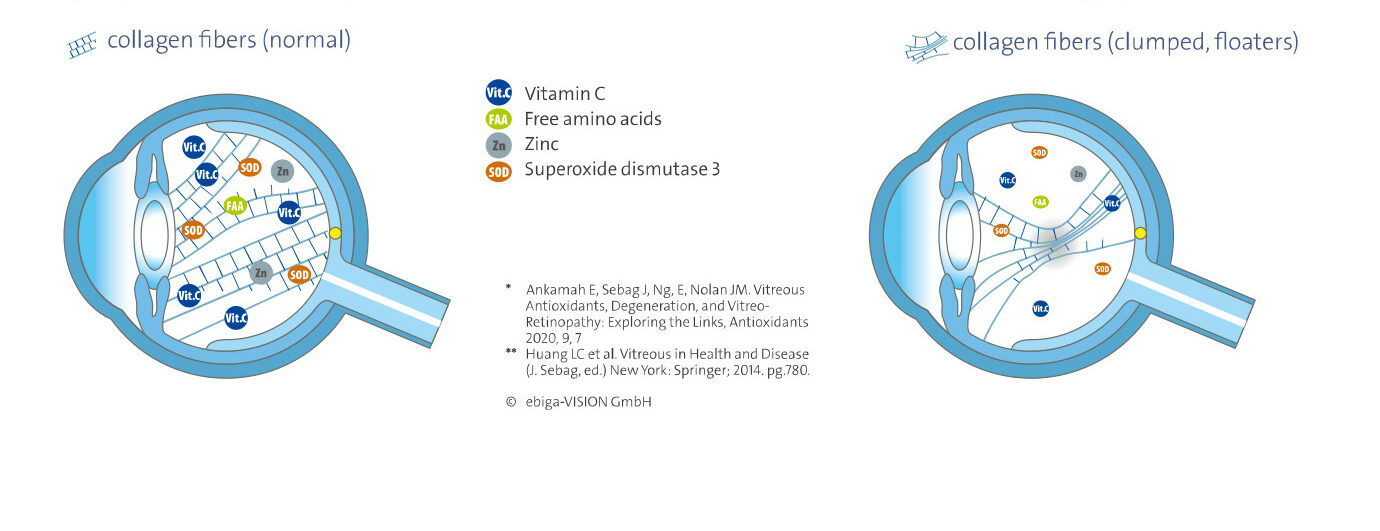
The vitreous body has a unique protective mechanism against >oxidative stress and >collagen glycation. However, this mechanism loses efficacy during degeneration. Providing the eye with naturally occurring micronutrients (vitamin C and zinc) and other micronutrients, can help reactivate this mechanism, minimizing or even preventing collagen fibers from clumping. The following micronutrients are known to accumulate in the human vitreous and decrease with degeneration and disease:
- Vitamin C helps counter intraocular oxidative stress by consuming >reactive oxygen species and >free radicals in an ascorbate-dependent manner.
- Zinc stimulates the synthesis of >metallothionein, a metal-binding protein that protects tissues from glycoxidation, thus exhibiting antioxidative and antiglycation properties. Zinc is also an important cofactor of >superoxide dismutase 3 (SOD3), a metalloprotein enzyme that catalyzes the dismutation of >superoxide radicals to hydrogen peroxide and molecular oxygen. Therefore, zinc also functions to regulate oxidative stress in the vitreous
- L-Lysine, an essential free amino acid helps prevent collagen glycation and serves as a >chemical chaperone.
Other micronutrients are known to effectively combat oxidative stress and protein glycation:
- Proanthocyanidins found in grapes has been shown to inhibit protein glycation.
- Hesperidin regulates oxidative stress and reduces the level of inflammatory cytokines by inhibiting the formation advanced glycation end products which enhances glycation of collagen.
Incorporating these micronutrients into one’s diet or through supplementation may potentially slow down or even reverse the progression of floaters, offering relief from the visual disturbances and emotional strain associated with this condition. >CLINICAL TRIALS have confirmed that a daily intake of 125 mg of l-lysine, 5 mg of zinc, 40 mg of vitamin C, 25 mg of proanthocyanidins, and 60 mg of citrus-flaminoids as hesperidin over a period of 6 months resulted in a reduction of vitreous opacity areas in 77% of the patients.
Risks and Suitability of Proactive Diet and Supplementation
For a comprehensive analysis of the benefits and drawbacks, refer to the article >How to reduce eye floaters naturally.
Atropine eye drops
Atropine eye drops are commonly used for various purposes in ophthalmology. One of their primary applications is to induce pupil dilation, which is useful for conducting eye examinations, particularly when examining the retina or conducting certain surgical procedures.
Researchers have been able to demonstrate a subjective improvement in floater symptoms in this context. This can be explained by the fact that the shadows of the opacities are less pronounced due to the increased influx of light. It’s important to note that Atropine eye drops are prescription-only, so they should be used under the guidance of a healthcare professional.
Risks and Suitability of Atropine eye drops
Atropine eye drops can alleviate the symptoms of vitreous floaters and thus provide a quick solution for patients experiencing significant discomfort. However, they do not address the root cause of the floaters. Additionally, their use for the treatment of floaters is not actually intended. The application leads to an artificial dilation of the iris and side effects such as disturbances in the eye’s focusing ability, increased sensitivity to glare, and occasionally inflammation of the eyelid margin and conjunctiva, resulting in eye burning, tearing, photophobia, and blistering.
Vitrectomy
Vitrectomy is a type of eye surgery that involves the removal of the vitreous gel from the eye, either partially or completely, which is then replaced with a synthetic substance such as a saline solution, gas bubble, or silicone oil.
Two three types of vitrectomy-procedures are commonly performed:
- Pars Plana Vitrectomy: This procedure involves making small incisions in the pars plana, a region of the eye situated between the iris and the retina. Pars plana vitrectomy is often used to treat conditions such as retinal detachments, diabetic retinopathy and macular holes. It may also be employed to remove larger or denser eye floaters.
- Anterior Vitrectomy: During an anterior vitrectomy, the surgeon removes the vitreous gel from the front portion of the eye, typically through an incision in the cornea or sclera. This type of vitrectomy is less common and is usually reserved for specific situations, such as addressing vitreous strands or debris during cataract surgery.
- Limited vitrectomy: This type of vitrectomy is performed using small-gauge instruments, typically with incisions less than 1 mm in size. Limited vitrectonomy is commonly used to address floaters while minimizing the risk of complications associated with traditional vitrectomy techniques.
Risks and Suitability of Vitrectonomy
Vitrectomoy allows for access to the retina and enables the surgeon to address underlying issues contributing to vision disturbances. It is primarily used to treat more serious retinal conditions; it has also been explored as a potential option for addressing bothersome eye floaters. The complete removal of the vitreous has a 100% success rate in eliminating eye floaters. However, its use for this purpose remains controversial due to associated risks and limitations.
Vitrectomy is a major surgical procedure that carries inherent risks, such as:
- Severe sight-threatening complications if the retina is damaged during surgery, including cystoid macular edema, epiretinal membrane formation, and retinal tears and detachment
- Infection and inflammation of the eyeball caused by the surgery
- Early cataract formation with potential loss of accommodation, often requiring a second surgical intervention to remove and replace the natural lens with an artificial lens
- Increased intraocular pressure
- Furthermore, the partial removal of the vitreous gel can potentially lead to the recurrence of floaters or the development of new ones.
Laser-Vitreolysis
Vitreolysis is a minimally invasive method for treating eye floaters using a YAG laser, a medical device that produces a high-energy laser beam. During laser vitreolysis, extremely short pulses of laser light are precisely directed into the vitreous body. The effect on floaters are:
- Fragmentation
- Displacement from the optical axis
The laser beam is precisely directed towards the affected area of the vitreous where large floaters are located and breaks large collagen conglomerates into very small ones that should no longer disturb vision.
Risks and Suitability of Vitreolysis
Despite its effectiveness, vitreolysis also carries risks. Serious complications, such as lens and retinal injuries, may occur. Therefore, doctors only perform this treatment after conducting a thorough diagnosis and providing comprehensive patient education. Additionally, this treatment can only be applied to large floaters, and only if they are located at a sufficient distance from the retina and the lens.
Renowned physician Dr. Karl Brasse categorizes floaters into 5 groups to determine the suitability for vitreolysis:
- Group I: Floaters originating from the retina opercula, usually well treatable.
- Group II: Floaters originating from the posterior border of the vitreous or from the vitreous cortex (Weiss ring), usually well treatable.
- Group III: Floaters within the vitreous tissue, only partially treatable.
- Group IV: Floaters originating from the back lens, usually well treatable.
- Group V: Various floaters from different causes such as inflammation, degeneration, injuries, rarely indicated for treatment.
It is important to note that when treating Group III floaters with vitreolysis, many small fragments may form, which tend to aggregate. Within a few weeks, new floaters may develop, which may be more bothersome than the original ones, particularly in the case of very large floaters.
General risks
- Lens hit with potential clouding of the lens and subsequently more difficult cataract surgery
- Retina hit with tissue damage to the retina and choroid (bleeding, secondary choroidal neovascularization)
- Increased symptoms due to the appearance of multiple small fragments
- Increased intraocular pressure